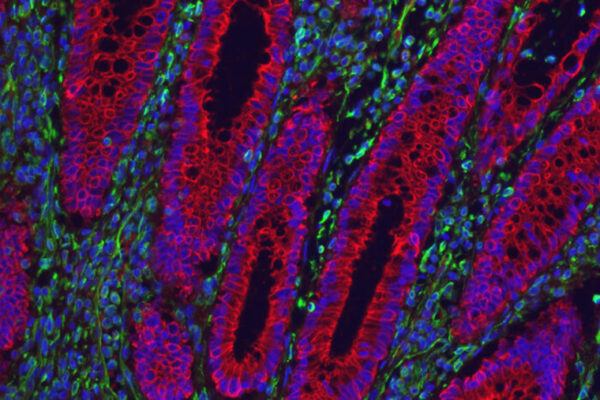
Inflammation and metabolic disorders are deeply intertwined. For example, people with inflammatory conditions such as Crohn’s disease and psoriasis are at risk of developing metabolic disorders such as insulin resistance and diabetes. However troubling that connection might seem, it also might point to some promising news.
Researchers at Washington University School of Medicine in St. Louis have received a Catalyst grant from the National Institutes of Diabetes and Digestive and Kidney Diseases (NIDDK) to investigate whether immunosuppressive drugs prescribed for inflammatory bowel disease (which includes Crohn’s disease and ulcerative colitis) or psoriasis also can control blood sugar levels. If they do, such drugs could provide a way to improve control of blood sugar in people with inflammatory diseases, thereby reducing the risk of serious complications such as diabetes. Catalyst grants are meant to support scientists of exceptional creativity who propose pioneering and possibly transformative approaches important to the mission of the NIDDK.
The idea for the study emerged from an unexpected observation. Gwendalyn Randolph, PhD, the Emil R. Unanue Distinguished Professor of Immunology and a professor of medicine, was investigating how people with Crohn’s disease handle fat in their diet by feeding participants a carefully designed milkshake and monitoring the levels of different kinds of fat in their blood over time. As part of the study, the researchers also collected data on blood sugar levels. The primary result of that study was negative: People with Crohn’s and healthy participants processed fat much the same. But an odd pattern in the data caught Randolph’s eye: The five Crohn’s patients who happened to be taking the anti-inflammatory drug ustekinumab maintained normal blood sugar levels after a meal, unlike other participants with Crohn’s disease who were taking other medications. Their glucose levels strayed higher and normalized more slowly than healthy controls.
“It was really just a side observation; the study was not designed to address the question of blood glucose levels,” said Randolph, the principal investigator on the $500,000 NIH grant. “But this new grant will help us check it out and see if it has merit. It’s an exciting hypothesis because people with inflammatory bowel disease (IBD) are at higher risk of developing metabolic disorders including type 2 diabetes, and there are not great medications to treat glucose problems linked to inflammatory disease.”
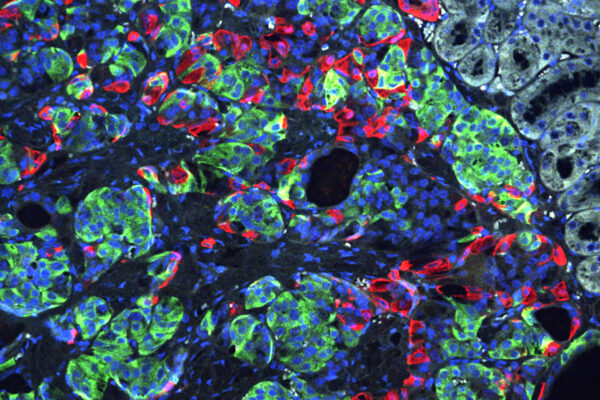
As a drug that might control blood sugar, ustekinumab may be a dark horse. Scientists have speculated for years that suppressing pro-inflammatory molecules known as cytokines might help control blood sugar in people with chronic inflammation. But there are dozens of cytokines, and none of them have panned out in clinical trials. The two cytokines suppressed by ustekinumab — IL-12 and IL-23 — have never been high enough on the list of likely targets to warrant a study.
The serendipitous observation suggests that IL-12 and IL-23 may have previously unrecognized effects that could shine light on the complicated relationship between metabolism and inflammation.
“We caught a glimpse of something, in the previous study, related to how metabolism is modified in the setting of inflammation,” said co-investigator Parakkal Deepak, MBBS, assistant professor of medicine in the Division of Gastroenterology. As a member of the medical faculty of the Inflammatory Bowel Disease Center, Deepak sees patients with IBD on the Washington University Medical Campus. “With further investigation into this area, we one day may be able to select therapy for people with inflammatory diseases based on the underlying metabolic profile and the effect of specific treatments on that metabolic profile.”
The researchers plan to study patients who have inflammatory diseases and already are taking drugs that target IL-12 or IL-23. With the help of the Center for Human Nutrition, the researchers will monitor levels of blood sugar and other biomolecules while participants are fasting and after meals. Bettina Mittendorfer, PhD, professor of medicine in the Division of Geriatrics and Nutrition Sciences and an expert on glucose metabolism, is helping to design the study in people.
The researchers also are planning mouse studies to see if neutralizing IL-12, IL-23 or both improves glucose and insulin tolerance.
“The implications are much larger than diabetes alone,” said co-investigator Matthew Ciorba, MD, associate professor of medicine in the Division of Gastroenterology and director of the IBD Center. “There are several other important complications of IBD linked to glucose metabolism, notably nonalcoholic fatty liver disease. Understanding if current therapies can modify glucose and other metabolic complications has the potential to impact millions of patients across the world.”
Washington University School of Medicine’s 1,500 faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is a leader in medical research, teaching and patient care, ranking among the top 10 medical schools in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.