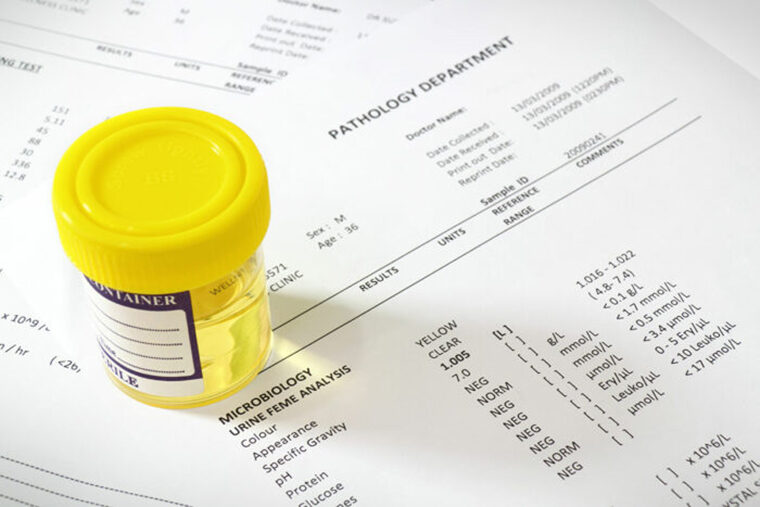
Tests to detect urinary tract infections (UTI) often are performed routinely in hospitals, even when patients don’t have symptoms. Such testing “just to be safe” can return results that lead doctors to prescribe antibiotics when there’s little to no evidence to warrant such treatment.
Now, new research indicates that making a simple change to the electronic system used by doctors to order urine tests can cut by nearly half the number of bacterial culture tests ordered without compromising the ability to identify people who need treatment for UTIs. The change encourages doctors to first look for signs of a UTI before testing a patient’s urine for bacteria.
The study, by a team at Washington University School of Medicine in St. Louis, is published Feb. 21 in Infection Control and Hospital Epidemiology.
“Over-testing for UTIs drives up health-care costs and leads to unnecessary antibiotic use which spreads antibiotic resistance,” said senior author and infectious diseases specialist David K. Warren, MD, a professor of medicine. “Ordering tests when the patient needs them is a good thing. But ordering tests when it’s not indicated wastes resources and can subject patients to unnecessary treatment. We were able to reduce the number of tests ordered substantially without diminishing the quality of care at all, and at a substantial cost savings.”
Bacteria in a person’s bladder can cause UTIs, which are characterized by burning or pain while urinating, frequent urges to urinate and fever. UTIs are treated with antibiotics. But some people – often elderly people or those with diabetes – harbor harmless bacterial communities in their bladders that do not need to be treated with antibiotics.
Before ordering a urinalysis to check for bacteria in the urine, infectious disease specialists recommend that physicians look first for signs of bladder infection using a urine dipstick test. This test can detect inflammatory cells in the urine – signs of a problematic UTI that may require treatment with antibiotics. Discovering bacteria growing in the urine without knowing whether the patient has signs and symptoms of infection leaves physicians uncertain of whether the patient will benefit from antibiotic treatment.
“Doctors get stuck with a result they don’t know how to interpret and often prescribe antibiotics because that seems like the safest path to take,” said Warren, who is the medical director for infection prevention at Barnes-Jewish Hospital.
Warren, first author Satish Munigala, MD, a data analyst in infection prevention, and colleagues made two changes to encourage more informative urine testing among their colleagues at Barnes-Jewish Hospital. First, they sent an email to all clinicians explaining the rationale behind ordering a urine dipstick test for signs of infection before ordering a bacterial culture test. Then, they changed the electronic ordering system. They set the default to a urine dipstick test followed by a bacterial culture test, rather than a culture test alone, which had previously been the first option. Clinicians who wished to order a culture test alone could still do so, but they had to open an additional screen on their computers.
The researchers compared all urine culture tests ordered at Barnes-Jewish Hospital in the 15 months before the intervention, staged in April 2016, to the 15 months after. Before the intervention, doctors ordered 15,746 urine cultures, or 38 orders per 1,000 patient-days. After, they ordered 45 percent fewer: 8,823 total, or 21 orders per 1,000 patient-days.
In particular, the number of urine cultures from people with catheters – who are at high risk of UTIs – dropped from 7.8 to 1.9 per 1,000 patient-days while the number of catheter-associated UTIs did not change at all. There were 125 diagnosed catheter-associated UTIs in each time period.
“Everyone always worries that by ordering fewer urine cultures we might miss some UTIs, but we showed that we did not,” Warren said.
Since it costs about $15 to perform a urine culture, the intervention saved approximately $104,000 in laboratory costs alone over the 15-month period. The researchers were unable to obtain pharmacy records to determine whether more careful testing decreased antibiotic prescriptions, but previous studies have shown that minimizing unwarranted testing does reduce antibiotic overuse.