Mice that sleep fitfully could help researchers unravel the mystery of insomnia.
Researchers at Washington University School of Medicine in St. Louis studied mice genetically modified to mimic the genetic disease neurofibromatosis type 1 (NF1), which is associated with sleep problems. They found that the animals, like some people with NF1, slept in short, irregular spurts. Studying these mice could help identify the molecular and cellular mechanisms that go awry and cause fragmented sleep patterns in people with and without the disease, the researchers said.
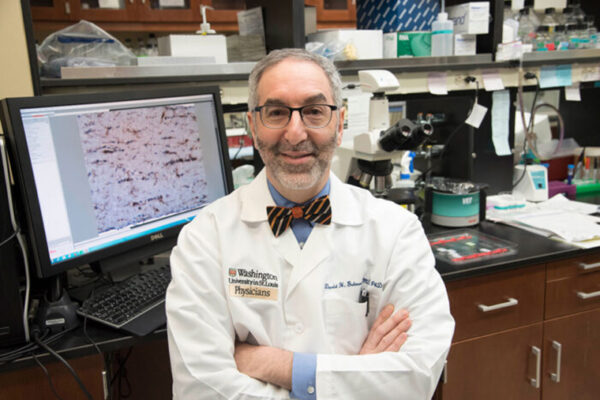
“The mice are a tool for us to understand how sleep disturbances arise and how sleep disruption contributes to problems with learning and attention,” said David H. Gutmann, MD, PhD, the Donald O. Schnuck Family Professor of Neurology and the study’s senior author. “This could apply both to people with NF1 and others without NF1 who also have sleep problems.”
The findings were published Jan. 4 in the Journal of Sleep Research.
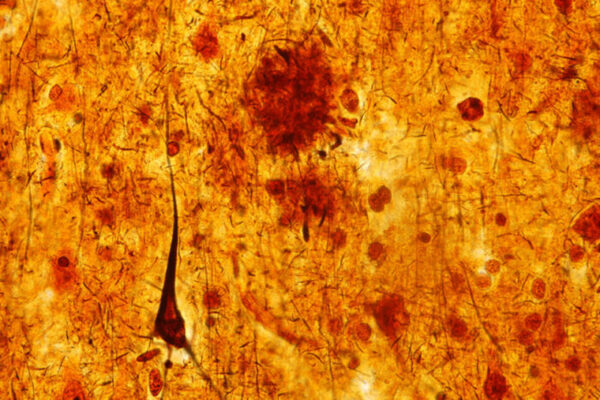
As many as half of people with NF1 – a condition that causes benign tumors in the brain and on nerves throughout the body – have difficulty falling or staying asleep. Learning disabilities and attention problems also are common in children with NF1, and both may be exacerbated by poor sleep. But doctors don’t know why some children with NF1 develop sleep problems and others don’t, nor can they do much to help them sleep better.
“Right now we just treat children and adults with NF1 and sleep problems like we treat patients without NF1 because we don’t understand what causes them,” said Gutmann, who also directs the Neurofibromatosis Center at Washington University.
Co-first author Corina Anastasaki, instructor in neurology, bred mice with a mutation in their Nf1 gene similar to what is seen in people with NF1. Then, co-first author Nicholas Rensing and Michael J. Wong, MD, PhD, the Allen P. and Josephine B. Green Professor of Pediatric Neurology, fitted onto the mice miniature versions of the caps people wear for sleep studies, enabling them to measure brain waves and identify sleep patterns.
Mice normally sleep during the day and, like people, cycle several times from deep, dreamless sleep to REM sleep – or dreaming – and back again. Mice with an Nf1 mutation, however, tended to wake up soon after they entered deep sleep. The result was a fragmented, and probably not restful, day of sleep.
“Throughout the whole night and day, they fell asleep and woke up when they shouldn’t have,” Anastasaki said. “They fell into deep sleep, but they didn’t stay there.”
Although the mice were engineered to mimic human NF1 disease, they could yield insights about the biological underpinnings of sleep in general, which could help people with sleep problems unrelated to NF1. About a third of American adults report some degree of insomnia, and 15 percent have chronic insomnia that lasts three months or more.
“It is hard to study sleep problems in people because there are so many factors that influence how well you sleep – maybe you’re stressed out, maybe you’re sick, maybe you’re taking care of a new baby,” Gutmann said. “But now we have a controlled system that we can use to start looking at which cells and proteins are involved, and which biological factors influence sleep quality. Only when we understand the problem better will we be able to find better ways to treat it.”