Two new studies explain why some parasite infections, such as those common in developing countries, sometimes can’t be cured with standard treatments.
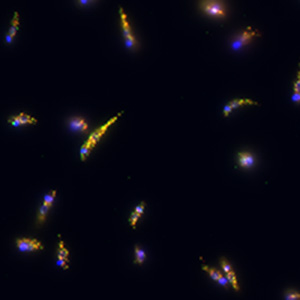
The research shows the parasite Leishmania — which infects 12 million people worldwide — often harbors a virus that helps the parasite survive treatments.
The findings, available online in The Journal of Infectious Diseases, suggest that simple changes in current treatments could improve the lives of millions of people sickened by parasite infections.
“Our findings may mean that treatment for Leishmania infections could be significantly improved by determining if the parasites are infected with a virus and modifying treatment accordingly,” said Stephen Beverley, PhD, senior author of one of the studies and the Marvin A. Brennecke Professor and head of the Department of Molecular Microbiology at Washington University School of Medicine in St. Louis. “In the future, it may be possible to improve the success rate of treatment by giving patients an antiviral medication as well as an antiparasite medication.”
Beverley and colleagues in Peru, Bolivia, Belgium, France and Switzerland studied the Leishmania parasite in three South American nations. Beverley’s team focused on infections in Bolivia and Peru, while the other team, led by Catherine Ronet, PhD, of the University of Lausanne in Switzerland, worked with colleagues studying patients in French Guiana.
Leishmaniasis is mainly spread by sand flies. Depending on the parasite species, symptoms of infection may include large skin lesions, fever, swelling of the spleen and liver, and sometimes disfigurement and death.
The virus carried by the parasite is called Leishmaniavirus, or LRV1. In earlier research in animals, the scientists found that Leishmania causes more severe infections when the parasite is infected with LRV1. This prompted the researchers to study the effects of the virus in people.
The Swiss team studied 75 patients in the small South American nation of French Guiana. Treatment failed among 30 percent of patients infected with Leishmania that carried the virus, but did not fail in any patients infected with parasites that did not carry the virus.
Beverley and his colleagues in Peru, Bolivia and Belgium examined data on 97 leishmaniasis patients. These were gathered through a project on drug resistance, funded by the European Commission and led by co-author Jean-Claude Dujardin, PhD, of the Institute of Tropical Medicine, Antwerp, Belgium.
“In Peru, leishmaniasis is common in people who work in agriculture and forestry,” said lead author Vanessa Adaui, PhD, of the Cayetano Heredia University in Peru. “Medical resources are often very scarce in the communities where these people work, and although infections typically are not fatal, they can lead to significant scarring, social stigmatization and economic loss.”
“All over the world, treatment failure is a major obstacle to the control of infectious diseases like leishmaniasis,” said Dujardin. “It is of uppermost importance to understand the factors contributing to this failure to better tackle it.”
The researchers found that treatment failed to cure more than 50 percent of patients with parasites infected with the LRV1 virus. But the failure rate was only 24 percent in patients with parasites that were free of the virus.
The standard treatment for leishmaniasis differs based on the parasite species that causes the infection and varies by location. In French Guiana, for example, patients are treated with pentamidine; in Peru and Bolivia, they receive a class of drugs called pentavalent antimonials. The modes of action of the two treatments are very different, according to Beverley.
“In the studies, different parasites were being pursued with different treatments, but the results were very similar: Parasites infected with the virus were harder to cure,” he said.
Based on the new research, it may be possible to develop clinical tests to identify virus-infected parasites. This could guide physicians in prescribing a combination of antiparasite and antiviral medications for patients with virus-infected parasites, improving the chances of successful treatment.
The scientists are investigating how viral infection makes leishmaniasis more difficult to cure. According to Beverley, the parasites infected with the virus may be interacting with patients’ immune systems in a way that disrupts treatment. Another, more likely possibility is that an increase in parasites spurred by the virus may make it more challenging for treatment to completely eliminate the parasites.
“A number of other human parasites bear viral infections that are reminiscent of LRV1 in Leishmania,” Beverley said. “If the viruses’ effects on these other parasites are similar, these findings may open the door to new approaches to treating a range of parasites in the future.”
This research was supported by the National Institutes of Health (NIH), grant number AID R56 AI099364; the European Commission (Projects LeishBolPe, Contract ERBIC18CT960123, and LeishNatDrug-R, Contract ICA4-CT-2001-10076); and the Directorate-General for Development Cooperation of the Belgian Government (Framework Agreement 03-project 95502).
Adaui V, Lye L-F, Akopyants NS, Zimic M, Llanos-Cuentas A, Garcia L, Maes I, De Doncker S, Dobson DE, Arevalo J, Dujardin J-C, Beverley SM. Association of the endobiont double-stranded RNA virus LRV1 with treatment failure of human leishmaniasis caused by Leishmania braziliensis in Peru and Bolivia. The Journal of Infectious Diseases, online June 29, 2015.
Washington University School of Medicine’s 2,100 employed and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient-care institutions in the nation, currently ranked sixth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.