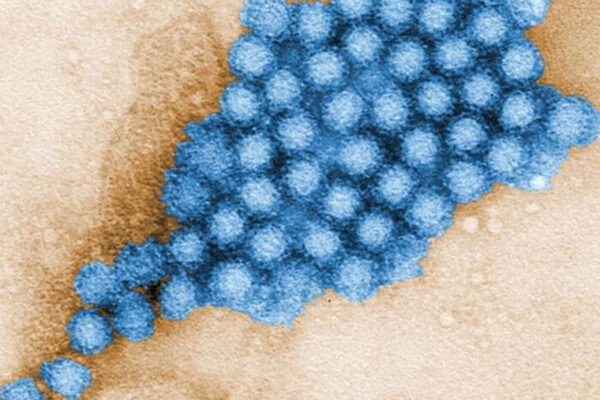
Antibiotics aren’t supposed to be effective against viruses. But new evidence in mice suggests antibiotics may help fight norovirus, a highly contagious gastrointestinal virus, report scientists at Washington University School of Medicine in St. Louis.
The researchers found antibiotics could help prevent norovirus infections. The same team also showed that a recently identified immune system molecule can cure persistent norovirus infections even in mice with partially disabled immune systems. The surprising findings, available online in Science, will appear Jan. 16 in the journal’s print edition.
Outbreaks of norovirus are notoriously difficult to contain and can spread quickly on cruise ships and in schools, nursing homes and other closed spaces.
The researchers found that norovirus works its way into gut tissue in mice that have been pretreated with antibiotics but that the virus cannot establish a persistent infection. Follow-up studies showed that norovirus needs a bacterial collaborator to establish a persistent infection in the gut. Eradicating the bacterial partner with an antibiotic can prevent persistent norovirus infection in mice.
“The virus actually requires the bacteria to create a persistent infection,” said senior author Herbert W. Virgin IV, MD, PhD, the Edward Mallinckrodt Professor of Pathology and head of the Department of Pathology and Immunology. “The virus appears to have a symbiotic relationship with the bacteria — they share the job of establishing persistence.”
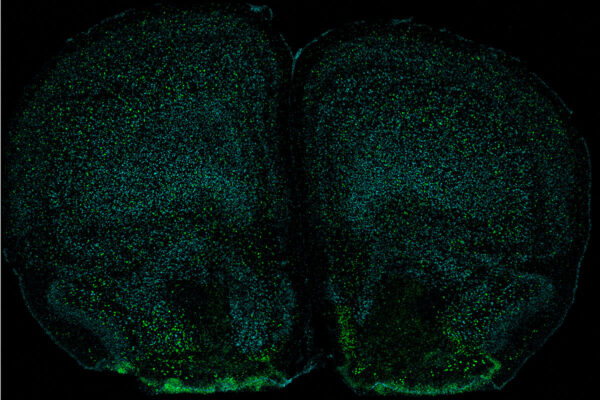
No studies have indicated that animals or insects carry and spread human norovirus. Therefore, scientists suspect that the sources of outbreaks may be people who have persistent norovirus infections but don’t have symptoms, such as stomach pain, nausea, diarrhea and vomiting. Virgin and his team decided to explore this possibility by studying a mouse model of chronic norovirus infection.
In additional tests, the scientists found they could restore the norovirus infections by transplanting fecal material from untreated mice into mice that earlier had been treated with the antibiotics. The transplants contained the bacteria eliminated by the antibiotics.
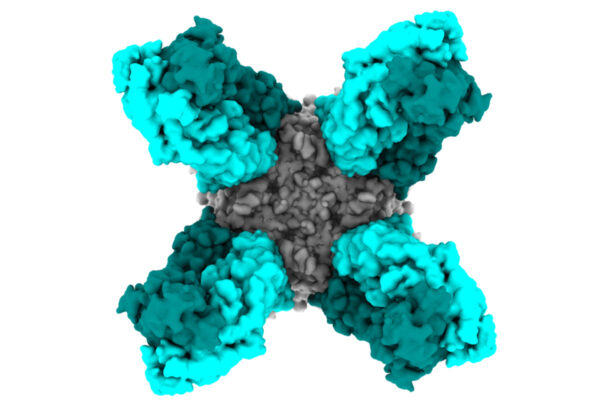
The scientists also looked for mouse proteins essential to preventing chronic norovirus infections. They found that a receptor protein for an immune inflammatory factor known as interferon lambda was required for antibiotics to prevent infection. Giving the mice interferon lambda also prevented norovirus infection, suggesting it also should be evaluated as a treatment for norovirus.
In the second study, the Washington University researchers reported that treatment with interferon lambda offers a significant advantage: It not only prevents the start of persistent norovirus infections but also eliminates established persistent infections. This was true even in mice lacking immune cells that scientists thought were essential to eradicating viral infections.
“I believe that’s a new concept in immunology,” said Virgin. “We thought that interferon lambda and other related molecules in the immune system could only contain viral infections until other parts of the immune system, including antibodies and T cells, finished the job.”
The researchers speculated that other viruses and bacteria may form similar symbiotic partnerships in humans.
“We need a much more detailed understanding of how antibiotic treatment affects the links among host, bacteria and virus,” Virgin said.
Nice TJ, Baldridge MT, McCune BT, Norman JM, Lazear HM, Artyomov M, Diamond MS, Virgin HW. Interferon lambda cures persistent murine norovirus infection in the absence of adaptive immunity. Science, online Nov. 27, 2014; in print Jan. 16, 2015.
Washington University School of Medicine’s 2,100 employed and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient-care institutions in the nation, currently ranked sixth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.