Diabetes researchers hoping to enlist the help of a protein targeted by cancer therapies have gained an important new insight into how the protein, known as mTOR, works in the pancreas.
Ironically, diabetes researchers are hoping to promote the capability of mTOR that oncologists want to shut down: its ability to cause cells to reproduce by dividing into copies of themselves. That capacity can be deadly in tumors, but Michael McDaniel, Ph.D., professor of pathology and immunology at Washington University School of Medicine in St. Louis, wants to use mTOR’s ability to make cells divide to maintain enough insulin-making beta cells in the pancreas to prevent diabetes.
“We’re working to increase beta cell mass and survival by appropriately activating mTOR,” McDaniel says. “This could be useful both for persons at risk of type 1 and type 2 diabetes and to sustain transplants in patients who already have diabetes.”
McDaniel and his colleagues published their results in a recent issue of The Journal of Biological Chemistry. They uncovered new details of how mTOR activation affects beta cell reproduction and found evidence that mTOR’s effects can both aid and adversely affect beta cells.
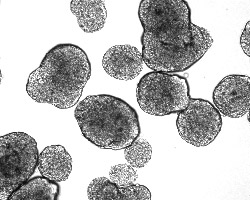
In earlier studies of rat islets, the structures in the pancreas that contain beta cells and secrete insulin, McDaniel’s group showed that glucose and other nutrients activate mTOR in the beta cells. They linked high glucose levels to increases in a beta cell’s production of DNA — a critical first step in the preparation for cell division.
Their experiments also suggested that glucose and nutrients activate mTOR by inhibiting potassium channels on the surface of islet cells and increasing calcium levels in the cell. Similar processes are involved in insulin secretion.
To further study the pathway activated by mTOR, scientists exposed the islet cells to glyburide, a compound known to inhibit potassium channels. It had similar effects, causing increased DNA synthesis through activation of mTOR.
Cells have to make a copy of their DNA to reproduce, but the fact that a cell is making DNA doesn’t guarantee that it will proliferate, moving all the way through the cell cycle and dividing into copies of itself.

When researchers studied how far beta cells went in the cell cycle when exposed to various levels of glucose, glyburide and an mTOR inhibitor, they found that chronic exposure to high levels of glucose or glyburide increased the number of cells in the DNA-making phase of the cell cycle. However, it also reduced the number of cells in the phase where cell division takes place. In other words, the cells were getting stuck in the DNA-making phase.
“We need to figure out what’s required to move cells to the cell division phase,” McDaniel says. “We may be missing some sort of cellular checkpoint here — another protein that’s a regulator of the cell cycle that is needed to move forward.”
Alternatively, McDaniel speculates that pulsed exposures to high glucose and nutrient levels that mimic daily feeding patterns could activate the mTOR pathway in a manner that causes beta cells to more consistently move beyond DNA synthesis and into proliferation.
Intertwined with the question of how to use mTOR to make more beta cells is the riddle of why beta cells become ineffective or die off in diabetics. McDaniel notes that beta cells in patients with uncontrolled type 2 diabetes also are exposed to chronic, high glucose levels.
“Other research groups have found evidence that when mTOR is overactivated, it activates a feedback loop that can increase insulin resistance,” he says. “We have also found this to be true in our system. It’s possible that further study of how mTOR responds to chronic, high glucose levels will give us important new clues about what’s going wrong in beta cells.”
Kwon G, Marshall CA, Liu H, Pappan KL, Remedia MS, McDaniel ML. Glucose-stimulated DNA synthesis through mammalian target of rapamycin (mTOR) is regulated by KATP channels. The Journal of Biological Chemistry, February 10, 2006, 3261-3267.
Funding from the National Institutes of Health, the American Diabetes Association and Takeda Pharmaceuticals supported this research.
Washington University School of Medicine’s full-time and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked fourth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.