Exercise may reduce more than your waist size. It also may help shrink a thickened and enlarged heart.
Researchers at Washington University School of Medicine in St. Louis have found that a moderate exercise regimen is just as effective as a common blood pressure drug in reducing the heart’s mass and the thickness of the heart wall in elderly individuals with mild to moderately elevated blood pressure. Both heart mass and wall thickness are potentially dangerous risk factors for future heart disease and heart failure.
Exercise also provided benefits that the heart drug did not, such as lowering an individual’s risk of developing diabetes. However, drugs still appear to be the best way to significantly lower blood pressure.
“Our study confirmed that medications are more effective than exercise in lowering blood pressure,” says principal investigator Ali A. Ehsani, M.D., a Washington University cardiologist at Barnes-Jewish Hospital. “But our main objective was to determine the effect of exercise on other important health factors such as heart size.”
The study was published in the August 2004 issue of the American Journal of Physiology: Regulatory, Integrative and Comparative Physiology.
Ehsani’s team randomly assigned elderly men and women to either medication or an exercise group. Those in the medication group received one dose of the common blood pressure drug hydrochlorothiazide once a day for six months.
Those in the exercise group underwent a two-phase training program. For one month, they participated in 40-minute flexibility classes three times per week. For the following five months, they did endurance exercises that incorporated brisk walking, jogging and/or cycling for 40 to 60 minutes three times a week. Initially, exercise intensity was about 60 to 70 percent of participants’ maximum heart rate, but intensity increased gradually to about 85 percent of maximum heart rate.
In both the exercise and medication group there were three participants whose blood pressure did not respond to treatment and who therefore were referred back to their primary care physicians for further treatment. A total of 28 volunteers who averaged 66 years of age completed the entire six months of the study — 16 in the exercise group, 12 in the medication group.

As expected based on previous studies, the medication was about twice as effective in lowering systolic blood pressure — the top number in a blood pressure reading. But the team found that exercise was just as effective as the drug in reducing other key health factors, such as the thickness of the heart muscle in the lower chambers of the heart, called the heart “wall.”
A key finding, according to Ehsani, was that exercise was as effective as hydrochlorothiazide in reducing the overall mass of the heart.
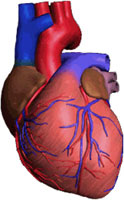
“One of the most dangerous effects of high blood pressure is its effect on heart mass,” he explains. “When you have high blood pressure, the heart has to work harder to pump blood to the rest of the body, which in turn results in a condition called hypertrophy, or an increase in the heart’s mass. Hypertrophy itself predisposes patients to conditions like heart rhythm abnormalities and can lead to heart failure.”
Ehsani’s team also evaluated the effect of the two treatments on metabolic conditions, such as resistance to insulin, which is a precursor to diabetes. Exercise significantly reduced insulin resistance and improved aerobic capacity, but hydrochlorothiazide had no effect on either.
“Based on our findings, my view is that patients with the early stages of high blood pressure should try to exercise and lose weight and see what happens,” Ehsani recommends. “If that doesn’t work, they need to be treated with medications. But it’s also possible that exercise and drugs have an additive effect in some people, and that some combination of the two will be the best option.”
Patients who would like more information can call 314-867-3627.
Rinder MT, Spina RJ, Peterson LR, Koenig CJ, Florence CR, Ehsani AA. Comparison of effects of exercise and diuretic on left ventricular geometry, mass, and insulin resistance in older hypertensive adults. American Journal of Physiology: Regulatory, Integrative and Comparative Physiology, v. 287(2), pp. 360-368, August 2004.
Funding from the National Institutes of Health supported this research.
Washington University School of Medicine’s full-time and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked second in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.


