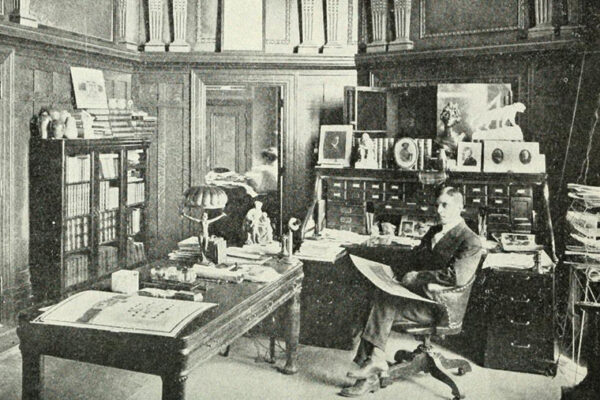
Trouble was brewing before the pandemic, according to Anthony Sardella, a senior research adviser at the Center for Analytics and Business Insights and adjunct lecturer at Olin Business School.
For years, the U.S. had become increasingly reliant on foreign manufacturers for chemicals and active pharmaceutical ingredients used in critical drugs like antibiotics, blood pressure pills, chemotherapy and cardiology drugs.
“Prior to the pandemic, the international supply chain was resilient enough to mask these concerns,” Sardella says. “But sudden changes in the supply chain and increased demand led to drug shortages that continue.”
Sardella’s research revealed the risks to our public health system created by overreliance on foreign manufacturers — noting that no manufacturing source exists in the U.S. for more than 83% of the active ingredients in the top 100 generic medicines, which represent over 90% of all medicines consumed.
The National Academy of Sciences cited Sardella’s research in its 2021 report to President Joe Biden, who made addressing this threat a key issue for his administration. Since then, the president has signed an executive order to launch the National Biotechnology and Biomanufacturing Initiative and pledged more than $2 billion for biotech and biomanufacturing efforts.
“By first leveraging existing manufacturers and, down the line, investing in additional facilities, the U.S. is on the right path to solidify and ensure the security of our drug supply chain.”
Anthony Sardella
The assumption had been that insufficient U.S. manufacturing capacity due to offshoring was largely to blame. However, in 2022, Sardella reported in “U.S. Generic Pharmaceutical Manufacturer Available Capacity Research Survey” that the U.S. does, indeed, have the capacity to make the nation’s most essential and critical drugs — yet most of the capacity is sitting idle.
Last year, the generic pharmaceutical industry made headlines when it announced the closure of several U.S. manufacturing plants, citing lower offshore operating costs and labor rates, intense pricing pressure and dependence on offshore sources for raw materials. Sardella and his team surveyed 37 of these sites and found that they are producing at only half of their annual capacity. Operating at full capacity would generate nearly 30 billion additional doses of essential drugs.
Sardella presented these results to industry leaders, government officials and the media last October at the National Press Club in Washington, D.C. He also proposed three recommendations: 1) create a public-private partnership model to reduce financial risk for U.S. manufacturers and make new technology available; 2) repurpose idle sites within 24–36 months; and 3) continue current federal funding efforts to ensure the economic sustainability of U.S. drug manufacturing.
One of the most significant and immediate developments to come out of the presentation is a new agreement to produce the chemotherapy drug lomustine — used to treat brain tumors, Hodgkin’s disease and other kinds of cancer — in the U.S. The agreement was made possible in part by API Innovation Center @ Cortex, a nonprofit Sardella founded in 2021 to coordinate efforts among manufacturers, technology innovators and government to produce drugs in the U.S. at lower costs.
“It’s enormous news for patients and their families,” Sardella says. “Lomustine will be manufactured for the Glioblastoma Foundation, which will provide it for patient care and clinical trials.”
Sardella says this is just one example of positive change ahead: “By first leveraging existing manufacturers and, down the line, investing in additional facilities, the U.S. is on the right path to solidify and ensure the security of our drug supply chain.”