In her course “Sick Society,” Hedwig (Hedy) Lee, professor of sociology, asks students to consider what aspects of our society impact our health. The answer is broader than it appears.
“If we want to understand what’s driving health, we have to look beyond what happens in the doctor’s office or the hospital,” Lee says.
There are social determinants to health. Those are things like your neighborhood, your housing, your education, your income, your job and your stress levels.

In the course, students define the nature of population health and study various populations and the issues surrounding their health, including people of different races, genders and sexual orientations; people with varying levels of education; and vulnerable populations such as children, undocumented immigrants and people in prison.
Income level, employment and circumstances determine a lot. A doctor may see a patient with hypertension and recommend exercise and diet modification. But the person may be a truck driver or working three jobs because a family member is incarcerated, making implementing these potentially beneficial changes difficult. Plus, “there’s research that shows chronic stress can lead to hypertension independent of changes in health behavior,” Lee says.
Our health, therefore, is influenced by nearly every aspect of our lives. And America has exceptionally bad health compared with other high-income nations. While a lack of universal health care plays a role, it isn’t the only factor in America’s health problems.
“In the course, we read a paper that compares millionaires in the United States to millionaires in other high-income countries,” Lee says. The expectation is that the millionaires are healthy because they can get the best health care, live in the best neighborhoods and eat the healthiest foods. “But we find that Americans have poorer health compared with other individuals of the same income. So students have to think about what the cultural and social features of our society are that might also be impacting health.”
Students also define what health is. “Does healthy mean the absence of any illness? Or is it about being able to live your life fully every day?” Lee asks. “Is health about mental and physical health? Should happiness be a part of health, or is not having a mental health disorder enough?”
Lee wants students to have an expansive view of health, so they will understand the importance of distal interventions. These policy interventions don’t seem related to health but can have a big impact on people’s well-being, such as housing policy, voting policy and criminal justice policy. At the end of the course, students have to make recommendations about health interventions that could be effective, and they often talk about distal interventions. Engineering students have proposed that hospitals be redesigned to be more accessible and address health-care disparities. Pre-med students have suggested how medical training can be improved. Others suggest better funding for schools or public transportation.
One issue that gets at the complex nature of social determinants is infant and maternal mortality rates. The United States has a high infant mortality rate compared with other high-income countries. In 2017, more than 22,000 infants (babies in their first year of life) died in the United States, for a death rate of 5.79 per 1,000 births. The infant mortality rate is nearly twice as high for Black mothers: 10.97 per 1,000 births.
“Infant mortality rates for Black mothers who have at least a college degree are similar to those for white mothers with only a high school degree,” Lee says. Typically, higher education levels lead to better health outcomes, for a variety of reasons, including higher income and better health literacy. While racial discrimination in health care could be part of the reason for this disparity, Lee encourages students to look “upstream” for solutions — that is, to look at what happened before the point of care that may be influencing these numbers.
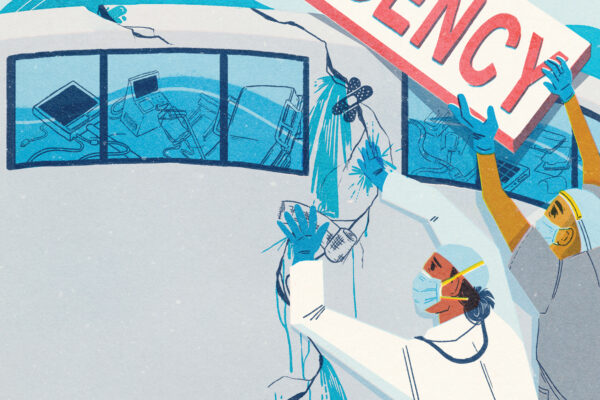
Anecdotally, doctors noticed emptier NICUs at the start of the pandemic. This could indicate that better maternity leaves might be an effective proximate intervention. (The most common cause of death for an infant in the United States is short gestation and low birth weight.)
Lee was not teaching “Sick Society” when the COVID-19 pandemic hit in the spring of 2020, but she taught it in the fall and added material to address the pandemic. Many of the issues around health disparities that COVID-19 has raised are familiar ones that the course already discussed. “COVID-19 has amplified how we think expansively about health,” Lee says.