Two people, facing each other, talking — let’s call it “excitedly” — are probably the most important ingredients for a debate. They are also a recipe for disaster if one of those two people has a highly contagious virus that has been shown time and again to be transmitted through the air.
Taking a cue perhaps from South Carolina Sen. Lindsey Graham’s Democratic challenger Jamie Harrison in an Oct. 3 debate, the vice presidential debate Oct. 7 features plexiglass barriers intended as a protective measure against the spread of SARS-CoV-2, the virus responsible for COVID-19. But it isn’t enough, counsels an aerosols expert.
“The shields are good if you have someone directly in front of you, and you are talking into it,” said Pratim Biswas, department chair and the Lucy & Stanley Lopata Professor in the Department of Energy, Environmental & Chemical Engineering at Washington University in St. Louis.
Otherwise, he said, particles just flow around them.
Biswas and researchers in his lab at the McKelvey School of Engineering have been using models to understand the different ways in which virus particles move around in a closed space.
 Their most recent efforts, led by doctoral student Sukrant Dhawan, show that — like putting up a plexiglass barrier — “common sense” solutions don’t always cut it when it comes to COVID-19. This is true particularly in a setting where an infected person and a non-infected person are facing each other, talking.
Their most recent efforts, led by doctoral student Sukrant Dhawan, show that — like putting up a plexiglass barrier — “common sense” solutions don’t always cut it when it comes to COVID-19. This is true particularly in a setting where an infected person and a non-infected person are facing each other, talking.
Plexiglass barriers won’t do much, but you also don’t need excessive distance between debaters. In fact, as long as the airflow is controlled, the safest distance between the two participants would be anything beyond about 4.5 feet.
This is one of a few surprises when it comes to what activities do — or don’t — carry high risk of infection.
“People say that speaking will not lead to airborne infection because the droplets emitted are lower in concentration than if you were coughing or sneezing,” Dhawan said. “But when you talk, you generally talk for longer periods of time.”
In fact, modeling shows that when standing about 8 feet apart, facing each other, the risk of being infected by a cough is less than 30%. At that same distance, there is more than a 40% chance of being infected by an infected person talking for a minute. And if they talk for 10 minutes, the risk is nearly 100%.
Certainly, that risk can be mitigated by airflow dynamics. “Wind blowing from an infected person is the most high-risk situation,” Dhawan said. Viral particles can travel farther, infecting the unsuspecting. “At least, that’s what we assumed initially.”
Yes, droplets can absolutely travel farther when carried by a wind, but they don’t stop when they sense the presence of a healthy person. They continue to whiz by.
“The faster the wind, the less amount of time you are exposed to the droplets,” Dhawan said. “Actually, increasing wind velocity decreases risk.”
Of course, the best case scenario would be to have the wind blowing from the uninfected person to the infected person. But what if you don’t know who’s who?
If wind velocity is about .5 meters per second in the direction of the person exhaling, these droplets can’t go further than 4.5 feet. “There is zero risk beyond that distance,” Dhawan said.
As long as the debaters are at least four and a half feet apart with airflow directed back at them (and a properly functioning air filtration system), the risk of infection is minimal to none.
With “common sense” leading us astray, however, and caveats upon caveats, it is reassuring to note that there is still one place in which common sense does intersect with reality for most of us.
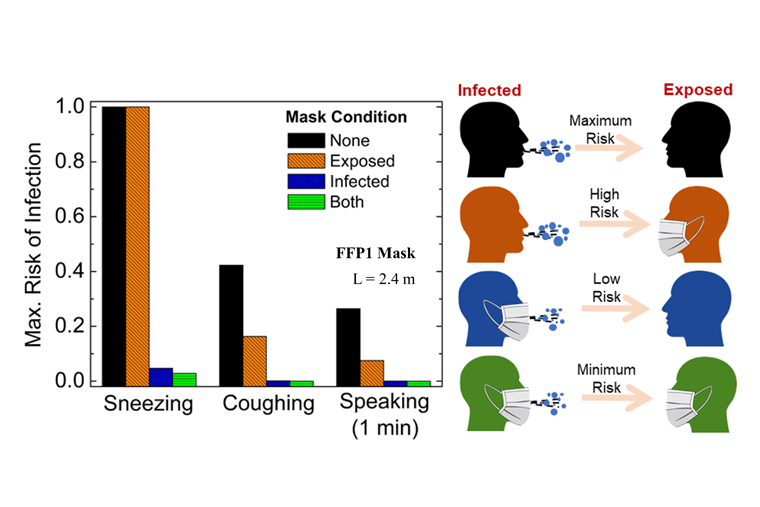
An infected person wearing a mask dramatically decreases the likelihood of infecting others.
In fact, at a distance of about 8 feet, an infected person coughing and speaking and, to a lesser degree, sneezing, is nearly as effective at preventing infection as if both people were wearing masks.
And since people infected with the SARS-CoV-2 virus do not always have symptoms, “the best thing, always,” Biswas said, “is to wear a mask.”