What infectious disease is deadliest worldwide? HIV? COVID-19? Malaria?
The answer is tuberculosis. And it kills more than 3,400 people across the globe every day — nearly 1.3 million in 2023 alone — and that number is rising fast. Without treatment, tuberculosis (TB) literally takes your breath away. Or it moves to your brain, lymph nodes, bones or kidneys — anywhere your blood can carry it.
Here in the United States, we think of TB as a relic of the past, a romanticized and tragic illness in which thin, flushed young women with sparkling eyes (they had a fever, for God’s sake) spat blood into lace handkerchiefs, said wan goodbyes and died. But TB is eradicated, right?
[TB] cases nationwide (though still few compared to the rest of the globe) are rising around 7% every year — with little public awareness of the resurgence.
TB did come under tighter control in the U.S. in the 1950s, thanks to public health efforts and the discovery of the antibiotic streptomycin. In the 1980s, Reagan-era public health cuts and the AIDS epidemic undid that progress, but by 1993, cases were again declining steadily, by about 7% a year. That lasted until 2020, when the COVID-19 pandemic artificially lowered the rate further because no one was getting diagnosed. But the lack of swift treatment helped TB regain momentum. Now, cases nationwide (though still few compared to the rest of the globe) are rising around 7% every year — with little public awareness of the resurgence.
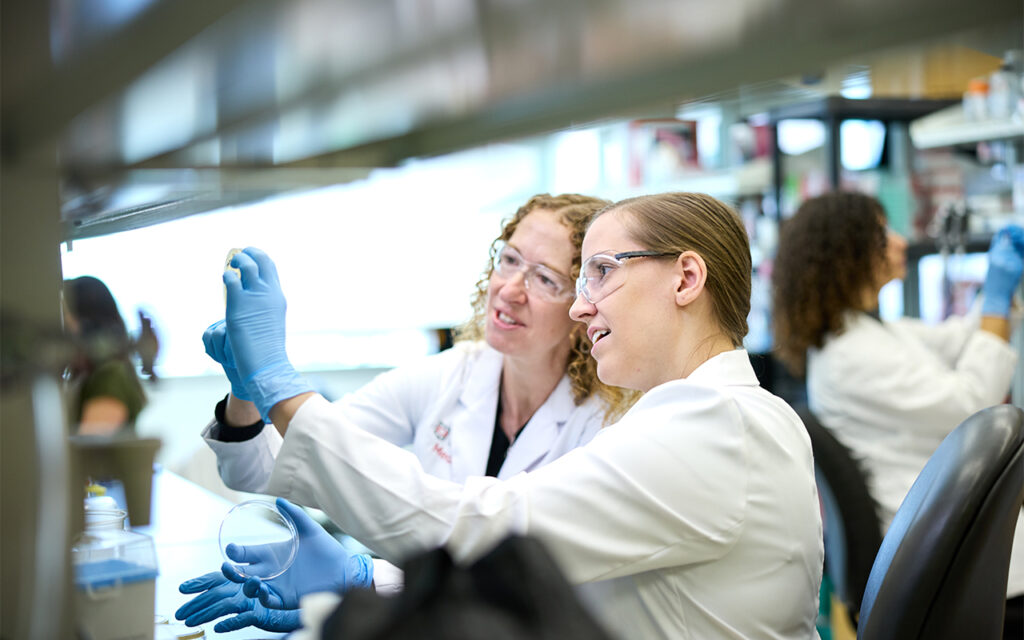
But that could change with a new WashU initiative — the Mycobacteria-focused Program for Research and Innovation in Science and Medicine (MycoPRISM) — that’s bringing together experts from multiple disciplines. From many vantage points, they will study TB’s causes and find new treatments. Meanwhile, the just-established School of Public Health, the university’s first new school in a century, will be looking at raising awareness and education, erasing stigma and addressing underlying causes.
Globally, there was a record number of new diagnoses in 2023 — about 8.2 million, the highest number since the World Health Organization began monitoring 30 years ago, according to the Journal of the American Medical Association (January 2025). And more than one-fourth of all living humans already have been infected. Often, Mycobacterium tuberculosis lies dormant, but any compromise to the immune system can spark it to life, even 80 years after someone is initially infected. And all it takes is one person with infectious TB to spread the disease. Across borders.
Why this is so tough to solve
When paleogeneticists broke open ancient mummies, they found them filled not with human DNA, which had degraded, but with tuberculosis DNA. TB is the disease that has proved immortal.
“TB has been infecting and killing people forever,” says Christina Stallings, PhD, a WashU Medicine professor of molecular microbiology and the Theodore and Bertha Bryan Professor of Environmental Medicine. “Yet, we still don’t have a hold of it. Why not?”
Because it is ancient, and it has coevolved with us. It’s had millennia to practice manipulating our immune system. Because it’s airborne, spread by the relentless coughs of people who are infected. Yet in a lab, it grows at a painfully slow rate, which makes it hard to study. Because we have no effective vaccine that protects adults from the disease.
In adults, TB generally hides in the lungs, where it can defend itself from the immune system. In children, whose immune systems are less developed, it travels to other sites in the body. Thankfully, a vaccine exists to protect children against severe complications. But, again, there is no effective vaccine capable of protecting adults from TB.
Because M. tuberculosis is so adept at defending itself, the standard treatment can take a full six months or longer. Four different drugs are used, a regimen designed to prevent the bacteria from developing resistance. But these antibiotics make some people sick, so they stop the treatment. Others feel better very quickly, so they stop the treatment.
“TB has been infecting and killing people forever. Yet, we still don’t have a hold of it. Why not?”
Christina Stallings, PhD
Still alive in the body, the bacteria can cause the patient to worsen or relapse. And if the drugs are not prescribed or taken correctly, the bacteria will develop resistance to the drugs, making the TB even harder to treat.
Even if a patient takes the full course of medication and improves, the bacteria might just find a quiet corner and go to sleep. “We have no way to know who actually clears it,” Stallings explains. “So it’s really hard to battle this pathogen when we can’t even tell who’s infected!”
In her lab, Stallings looks for ways that M. tuberculosis defends itself against the immune system and survives antibiotic treatment. What distinguishes mycobacteria, a subset of microbacteria, is that they are encased in an envelope waxed slick by fatty mycolic acids. That coat is disguise as well as armor: It can actually trick the immune system into aiding and abetting a pathogen it should have killed on sight. And if that doesn’t work, TB has learned other ways to survive an attack.
Enter the mice.
TB can infect any warm-blooded animal — two elephants at the Saint Louis Zoo, for example, have been diagnosed in the last 15 years. “They’re fine; they were very good at taking their antibiotics,” Stallings reports. “But it’s the mice we’ve learned so much from.
“We have this important immune cell in our bodies called a neutrophil … And what we discovered is that the neutrophils, instead of killing the bacteria, are actually promoting their ability to cause disease.”
Christina Stallings
“We have this important immune cell in our bodies called a neutrophil,” she continues. “Our blood is full of them, and anything that tries to invade us, they kill and eat. When we looked in the lungs of patients with TB, there were lots of neutrophils there eating the TB — but the people were still sick. We saw the same thing in our mice. And what we discovered is that the neutrophils, instead of killing the bacteria, are actually promoting their ability to cause disease.”
A neutrophil has an arsenal of weapons, and one is an extracellular trap. “Imagine an adorable round cell spitting out a spider web covered in deadly things,” Stallings says. “That web is meant to capture whatever it’s trying to kill — but mycobacterial TB has found a way to thrive on those deadly nets. It loves them. So we’ve been able to block the neutrophil’s ability to make that net.” Luckily, drugs were already being developed to do just that, because the nets also cause problems with arthritis and autoimmune disorders. “We hope to be able to use the same drugs to treat TB.”
She can’t pause to savor that success, though; far more needs to be discovered. And meanwhile, a new problem is emerging: Other mycobacteria, found naturally in the soil and water, are causing diseases that are even harder to treat. “They have acquired the ability to cause lung infections in patients who have declined lung function or are immunocompromised,” she explains. “They generally cause infections only when someone has an underlying condition, but when they do cause infection, it’s even harder to treat.”
Mycobacterium abscessus is one of them, and easily the worst. Those most affected are patients with cystic fibrosis, and sometimes the infection is untreatable. Stallings draws a deep breath. “It’s terrible. And the prevalence of these bacteria is increasing.”
Why now? “It’s not completely clear,” she says. “But Fangqiong Ling (an assistant professor in energy, environmental and chemical engineering in the McKelvey School of Engineering) is looking at the environmental reservoirs,” areas of water or soil where they thrive.
This kind of collaboration will be far more frequent, thanks to the MycoPRISM initiative. As co-director, Stallings is pulling together experts: “A lot of people at WashU are interested in mycobacteria — clinicians, basic science researchers, chemists, engineers, public health experts — but we were all functioning on our own in little pockets.” Compare notes, and you can build a world-class nexus of expertise.
Changing the face of the epidemic
The initiative’s other co-director is Jennifer Philips, MD, PhD, a WashU Medicine professor of medicine and of molecular microbiology, and co-director of the Division of Infectious Diseases. She, too, holds the Theodore and Bertha Bryan Professorship of Environmental Medicine. And her lab is looking at a different piece of the immune system. TB is canny, but if we shore up our defenses, that could help us avoid drug resistance and shorten treatment. “If it took two weeks instead of six months to treat TB,” Philips says, “that would change the face of the epidemic.”

At the moment, Philips is focusing on the interaction between TB’s lipids and the immune system’s macrophages, another type of cell that’s designed to kill and clear bacteria but fails miserably with TB. There are several types of macrophages, and TB has a different arsenal to combat each one. How do we best fight back?
She’s also studying the immune system’s T cells, which help make macrophages lethal to invaders. How can we strengthen that interaction? And she’s looking at cholesterol, which TB takes from its host for nutrition. “TB modifies cholesterol,” Philips says, “in a way our body does not. We think it does this to alter the immune response. We want to understand that mechanism.” Also, because the modifications could be detected in the blood, they could give us a new way to diagnose TB. A blood test would be easier and might be more revealing than a sputum sample. And the easier we can make diagnosis and treatment, the better we can control TB’s spread.
The challenges to public health
Diagnosing TB and controlling contagion are the purview of Thomas Bailey, MD, a WashU Medicine professor of medicine and medical director of the General Infectious Diseases Clinic, and medical director of the TB prevention program for the St. Louis County Department of Public Health. When a WashU Medicine doctor at Barnes-Jewish Hospital wonders if a patient might have TB, Bailey is consulted. When someone walks into the county health department with symptoms, Bailey takes sputum samples and gets the results of a molecular test back in a day or two, identifying not only the presence of infection but also any mutation on the TB gene that signals resistance to antibiotics.
“Many of these people have seen multiple doctors,” he says, “because TB is in such small numbers here that it’s possible to complete medical training without ever having seen a case.” This makes diagnosis trickier — especially with TB that occurs outside the lungs, as happens in 15% of cases.
“You breathe it in, the organism multiplies, and before the immune system can stop it, it has disseminated throughout your body — in a process that’s entirely asymptomatic,” Bailey explains. A patient’s chest X-ray may be completely normal, because the TB there has resolved, but it has gone on to the brain or bones.
It’s hard to convey urgency, Bailey says, because TB is uncommon in the U.S.: “about 10,000 people a year, compared to a worldwide incidence that’s close to 11 million. And about three-fourths of the people with TB in the U.S. were born outside the country.”

There are other risk factors, though. TB has risen all over the world since the pandemic. Both the SARS-CoV-2 virus and the drugs used to treat it had the effect of suppressing the immune system, making people more susceptible to TB. At the same time, the health-care system was overwhelmed, so public health resources were being pulled from TB to fight COVID-19. And people were afraid to seek treatment for a little chronic cough. Or drenching night sweats. Or, as time went on, the blood they were coughing up.
Since the pandemic, TB cases are rising by at least 7% a year — in a maddening coincidence, at the same rate they previously had been falling. In 2023, the U.S. had 9,600 cases; in 2024, the caseload rose to 10,300. The highest numbers are in populous California, Texas, New York and Florida; Missouri has a low prevalence, only 74 cases in 2023 and 85 in 2024. So it came as a jolt when cases in Kansas rose from 46 in 2023 to 115 in 2024, a 150% increase.
The Kansas outbreak, with cases clustering in Kansas City, was seemingly an anomaly — but there will be more and more anomalies.
“If we’re ever going to eliminate TB, and we still talk about it, we will need an adequate vaccine.”
Thomas Bailey, MD
“If we’re ever going to eliminate TB,” Bailey says, “and we still talk about it, we will need an adequate vaccine.” He sighs. “It took a lot of money and resources to get TB back under control in the ’90s. The standard of care became directly observed therapy, which is resource intensive.” Since studies showed that only about 11% of patients were completing the six-month therapy, health department staff have been literally watching people take their medication. (Now, there’s a secure app where patients can videorecord their doses.)
Between 2003 and 2016, to save money and improve compliance, public health experts tried to shorten the duration of therapies and even suggested that antibiotic dosing two to three days a week could be effective. “It took many years,” Bailey says grimly, “to figure out that there was an unacceptably high rate of relapse.”
Not only does TB’s treatment course need to be long, but it could take up to eight weeks just to culture a sputum specimen. Allison Eberly, PhD, is a WashU Medicine assistant professor of pathology and immunology and one of the medical directors of the clinical microbiology lab.
For the past decade, molecular testing has made a huge difference, but she still checks on the cultures for as long as 56 days, “because no test is perfect.” She also must send samples to a public health lab, because their advanced molecular techniques and sequencing can detect antimicrobial resistance.
What she finds about 10 times more often than TB, though, are the other mycobacterial infections Stallings referenced. What’s needed is a molecular test that can detect those infections, so patients can receive a faster diagnosis.
“No company has a commercially available test to identify non-TB mycobacteria,” Eberly says. When a sputum sample comes in, she does a stain, then a TB molecular test, and then she must wait until the isolate grows. Some mycobacteria grow faster than TB, but others take the full eight weeks. Once there is colony growth, she can use the mass spectrometer to identify which of the more than 200 species of mycobacteria she’s dealing with.
Because non-TB mycobacterial infections are not reportable diseases in many states, it’s hard to track the rate of infection. But, like TB, most of these infections require a three- to four-drug regimen and take months or years to treat.
The stigma of contagion
Not only do people with TB hate the six-month course of antibiotics and their side effects, but they also don’t want to admit they have the disease. Why is there still stigma, in this modern age? Because it is scary, contagious and chronic. Because it can remain in your body forever, and the treatment, at least in the U.S., is intrusive, with health department staffers showing up like Mary Poppins to watch you take your medication. And because the 19th-century romance is over: TB is now perceived as a disease of the poor.
Those most at risk for TB, of course, are people whose immune systems are compromised. Maybe they are taking a biologic for rheumatoid arthritis or some other autoimmune disease; or they are HIV-positive, elderly or underweight; or they smoke, have diabetes, or have a head, neck or gastric cancer; or they are receiving an organ transplant; or their kidneys are failing. But the most common risk factors are the usual enemies of health: malnutrition; overcrowding; homelessness; substance abuse; and lack of access to, or distrust of, health care. “TB is both a form and expression of injustice,” writes John Green in his sensitive and thorough New York Times bestseller, Everything Is Tuberculosis.
“TB is a disease of low-income countries predominantly. And we live in a world that neglects people who have fewer resources and less power.”
Sandro Galea, MD, DrPH
The dean of the new WashU School of Public Health, Sandro Galea, MD, DrPH, sees TB as an important disease that students should learn about as part of a comprehensive public health curriculum. Issues such as awareness, how to combat stigma, improve diagnosis and access to treatment, persuade people to finish their treatment, and tackle the underlying social forces that put them at risk are core to public health and important for all students to understand well.
“TB is a disease of low-income countries predominantly,” Galea says. “And we live in a world that neglects people who have fewer resources and less power.” That said, we also live in world where “TB is not going to respect borders. It’s going to grow.” Travel itself is a risk factor, especially to areas where TB is prevalent, and that list includes parts of China and India, the rest of South and Southeast Asia, Africa, Eastern Europe, the Caribbean, Latin America, the Middle East and the Pacific Islands.
The funding dilemma
Before the federal government’s USAID cuts, the global TB response was already about $11 billion short of the funding needed to control infection, Stallings says. Now, USAID is unable to distribute antibiotics to treat TB, which means more death and more contagion — which will be followed by even more death and even more contagion. Shipments of antivirals for AIDS have also been stopped, which means even greater susceptibility to TB, because an immune system needs the T cells being decimated by AIDS to fight TB.
“My entire lab runs on federal funding,” Stallings says, her voice tense. “We’ve already had a couple of grants delayed that were going to start March 1, to develop new antibiotics. We team up with Fimbrion Therapeutics (whose chief scientific officer Thomas Hannan, DVM, PhD ’08, is a WashU alum) to translate what we’re doing in the lab into treatments. Fimbrion has been developing these drugs, and they’re working fantastically. The grant would get them into clinical trials — but the funding is stalled.”
Bailey can already hear the arguments for cuts: “‘It’s just 10,000 people a year, so why do we need so much money to take care of them?’ Believe me, it’s not to pay health-care workers’ extravagant salaries,” he stresses. “The people I work with at the health department are almost saintly. They treat patients as they deserve to be treated, and they get paid very little. Some have more than one job.” Public health expenses could be responsibly lowered if we had an effective vaccine, but some big federal grants for vaccine development at other institutions are scheduled to be cut.
By investing in basic research, drug development and public health, the U.S. has been able to control a disease that runs rampant in other parts of the world, Bailey points out. Once TB spreads that far, even the best public health efforts are overwhelmed. “A country like India has so many cases, it can’t possibly hope to have TB under control, especially without an effective vaccine.”
“When you underinvest in public health, there’s a surge in illness … and that’s exactly what we’re heading into right now.”
Sandro Galea
Galea once co-authored a study that measured the effects of decreased public health funding after New York City’s 1975 fiscal crisis and the Reagan-era federal budget cuts. The findings were published in the American Journal of Public Health, and the accompanying graph tells the story: The incidence rate of TB begins to rise sharply after the cuts, drawing a mountain that peaks in 1993 before finally beginning to descend again. HIV and other public health dangers also rose after the cuts. Overall, the downsized budget initially saved New York City $10 billion — but ultimately cost the city more than $50 billion.
“When you underinvest in public health, there’s a surge in illness,” Galea says now. “New York had an enormous explosion, and that’s exactly what we’re heading into right now.”
The upshot
In the last five to 10 years, “we have learned so much about how TB infection progresses, its pathogenesis, how it causes disease,” says WashU Medicine’s Philips. Now, she stresses, we need an effective vaccine. We need more strategies and treatments that can disable TB, outwit multidrug-resistant TB, and strengthen and redirect the immune response. We need to understand what reactivates latent TB. And we need to raise public awareness of the deadliest disease in the world.
“With USAID efforts shuttered, we will see the numbers continue to increase — and that will inevitably spread to this country.”
Jennifer Philips, MD, PhD
“If we are lucky,” Bailey says, “and scientific investigation is allowed to continue, and we don’t completely destroy people’s faith in vaccines” — we can keep control, at least in this country. “But TB is a disease that’s highly adapted to humans. If you take your eye off the ball…”
Stallings echoes his worry. “TB has evolved with us — and it evolves faster than we do. We have got to find ways to stay ahead.”
If we don’t? “With USAID efforts shuttered, we will see the numbers continue to increase — and that will inevitably spread to this country,” Philips says.
Already, the death toll is rising, Galea adds. “We could certainly see a return of TB in this country.”