A researcher comes up with a great idea — software that lets you see the heart differently, a mesh that can heal wounds, a rapid test for heart attacks. So, now what?
It may seem straightforward — get the idea “out there.” But how exactly is that accomplished? At Washington University it’s through the Office of Technology Management (OTM), which guides innovators through the process of licensing intellectual property, launching startups, finding funding, filing patents and executing anything else necessary to bring an innovation to the marketplace.
“University technology can linger on the vine and die there, and it shouldn’t,” says Nichole Mercier, assistant vice chancellor and managing director of OTM. Under her leadership, OTM has sharpened its focus on customer service, connected more with innovators to find out about new discoveries, and created Quick Start Licenses that can get technology licensed in as little as 30 days.

“My vision is to define how we can pair cutting-edge university research with expertise and exceptional customer service from my office in order to create a pipeline of opportunities that can be beneficial to society,” says Mercier. Here is what happens when great ideas have a well-run innovation pipeline.
Mapping the heart
In summer 2015, Jon Silva, PhD ’98, associate professor of biomedical engineering in the McKelvey School of Engineering, was invited to the Microsoft campus to learn about the company’s latest tech. One item was the HoloLens, a mixed-reality headset that allows the wearer to see holographic images while still being able to observe the room around them.
“That has potential,” Jon thought and called his wife, Jennifer N. Silva, MD, associate professor of pediatrics in the School of Medicine. He asked her if it would be helpful to see the heart in three dimensions instead of the typical two when she treated patients with arrhythmia.
Jennifer was immediately enthusiastic. As a physician, she works in an electrophysiology cardiac catheterization lab. With the catheter, she maps out where the heart’s electrophysiological abnormalities are by creating two 2D images that she must then interpret to decide whether to surgically remove tissue. It can lead to a lot of mental fatigue.
“But we weren’t thinking, ‘let’s make a commercial tool,’” she recalls. “We just thought, ‘Wouldn’t it be great if we could do this?’”
The Silvas were the perfect team to tackle the project. The two met while working in the lab of biomedical engineer Yoram Rudy, the Fred Saigh Distinguished Professor of Engineering, who studies the heart. Jon was working on the data, doing computational modeling of molecules. Jen was looking at the whole heart, working on a noninvasive way to do electrocardiographic imaging — which led to the creation of the CardioInsight mapping vest (see sidebar below).
Despite both being interested in the electrophysiology of the heart, they had never found a project that dovetailed so perfectly with both their expertise.
Over winter break in 2015, Jon started working on software prototypes, which used catheter lab data to make a 3D image in the HoloLens. While gathering the data, Jennifer talked to some of her medical colleagues about the idea.
“They told me, ‘Stop talking. Go write a patent!’” Jennifer recalls. So she and Jon went to the Office of Technology Management.
The staff there helped them file a patent, using outside patent attorneys to draft the patent application. “What was exceptional about our colleagues at OTM was they taught us along the way,” Jennifer says.
With OTM’s help, the Silvas learned they’d need to form a company and were introduced to early funders. They connected with the Skandalaris Center and competed in LEAP: Leadership and Entrepreneurial Acceleration Program, a pitch competition that awards grants of up to $50,000 to advance university intellectual property toward commercialization. And LEAP participants get training on how to pitch investors.
Armed with their new skills, the Silva’s won that grant and several others, including funding from the Children’s Discovery Institute, which allowed them to launch their company, SentiAR, in 2017.
The SentiAR technology is considered a class 2 medical device, more complex than sunglasses (class 1 device) and less complex than a pacemaker (class 3). It requires approval by the FDA, and the Silva’s were able to get a $2.2 million grant from the National Institutes of Health and another $2 million from Venture Fund in St. Louis to go through the approval process. After two years in summer 2019, physicians were testing the SentiAR system in the lab for the first time.
“That was so exciting,” Jon says. “And in the early returns that we’re seeing, the physicians are getting their catheters to a better place, and the data reflect they have an easier, quicker understanding of what’s going on in the heart.”
(The Silvas will discuss the development of SentiAR and their software in a virtual event on June 18.)
Advancing wound care

When Joe came to BJC, he’d already had an open wound on his leg for more than a year. Joe had acquired it while battling head and neck cancer when doctors harvested bone from his leg to reconstruct his jaw. Though small, the wound was a plague. He had to bandage it every day and was constantly worried about infection. He couldn’t swim with his children, and it interfered with his career as a parole officer.
BJC was his last hope. But after seven surgeries, his wound was still not healing properly.
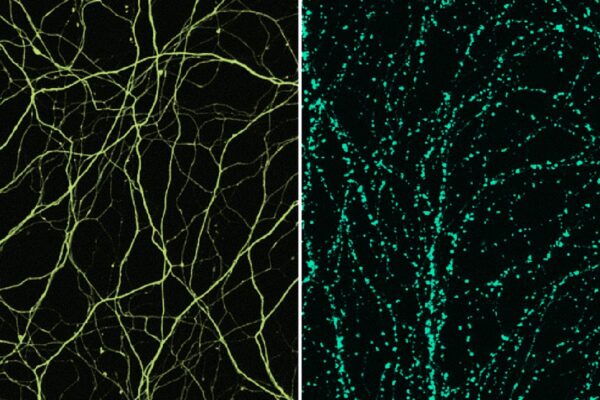
Fortunately, down the hall from his surgeon’s office was Matthew MacEwan, MD ’08, PhD ’18, who had developed a new technology capable of treating chronic wounds. As a graduate student, MacEwan had discovered that nanoscale materials could restore damaged tissue and heal difficult wounds. He took resorbable polymers, materials capable of dissolving in a patient’s body, and built matrices of nanoscale fibers on them that served as a scaffold for native cells to grow. MacEwan’s product, Restrata Wound Matrix, was ultimately used to successfully close Joe’s wound.
The discovery that led to this healing happened almost by accident. While earning his PhD in biomedical engineering at WashU, MacEwan worked next door to a lab where researchers were synthesizing various nanoparticles and nanomaterials. Intrigued, MacEwan wanted to see how they could be used in regenerative medical applications.
“That’s really what led to some of our initial discoveries around the biological potential of these nanofiber materials, and eventually the formation of the company,” MacEwan says.
In 2013, MacEwan founded Acera Surgical, while he was still a graduate student. His first product was a nanoscale material designed to repair the membrane around the brain and spinal cord, Cerafix Dura Substitute, which he made in conjunction with Washington University neurosurgeons. When Cerafix was approved by the FDA in 2016, it became the first nanofabricated surgical material approved in the U.S. Using the same technology, MacEwan designed Restrata for soft-tissue repair and Covora for partial-thickness burns. Today, MacEwan’s nanofiber technology is being used across the country in academic, commercial and VA hospitals. The materials offer an alternative to costly animal- and human-tissue products.
MacEwan gives a great deal of credit to the university for helping him through the process of bringing his technology to market.

“WashU is an amazing ecosystem,” MacEwan says. “There are so many talented individuals who are willing and excited to help develop new ideas and find new ways to improve human health. That includes in the Office of Technology Management, where they help make innovations into businesses. I’m positive that our connection to WashU, OTM and to St. Louis was critical to the success of our business.”
Testing a broken heart
The Office of Technology Management is not new to the university. Back in the early 1980s, Jack Ladenson, the Oree M. Carroll and Lillian B. Ladenson Professor of Clinical Chemistry, had a problem OTM helped him solve: angry clinical fellows and stressed lab techs.
Ladenson is a pathologist, and at the time the blood test (CK-MB, or creatine kinase MB isoenzyme) to determine if a patient had had a heart attack, or myocardial infarction (MI), took three hours to complete. The problem? New drugs to break up blood clots and re-establish blood flow needed to be administered within four hours of the onset of the MI.
“I’ve never seen such strained relationships between the laboratory and a clinical service,” Ladenson says. “And you couldn’t just blow it off, because it was real. It was pressure.”
Ladenson set out to find a way to get faster test results. With funding from Monsanto, his lab discovered two monoclonal antibodies — antibodies from a cell line made in labs that react to the presence of selected proteins in the blood, in this case CK-MB, which is released by the heart into the blood when an MI occurs.
“It was a faster way to measure if a person had suffered a heart attack, and that speed led to a greater degree of clinical success,” Ladenson explains.
When Ladenson presented his findings to Monsanto, it filed for a patent, but then returned rights for the discovery back to the university. Ladenson wasn’t sure what to do next, so he went to the university’s Office of Technology Management, which at the time had only one full-time employee, Duke Leahey, who helped Ladenson license his discovery.
Dade (now Siemens), the first health-care company to market Ladenson’s test, also funded more research. So Ladenson kept working on an even faster test and, with help from WashU’s cardiology division, came up with two.
“That’s what makes this university,” Ladenson says. “You’re able to cross departments and work together.”
One test, which detected the protein Troponin-I in the bloodstream, has become the gold standard for heart attack tests for its rapidity and accuracy and is still used today.
For Ladenson, the discoveries have led to many awards, including being named a National Academy of Inventors Fellow, the highest professional distinction accorded solely to academic inventors, as well as the inaugural Distinguished Award for Contributions to Cardiovascular Diagnostics from the International Federation for Clinical Chemistry in 2017. Further, the licensing fees he’s received for his monoclonal antibodies have allowed him to establish three endowed professorships in the School of Medicine.
And OTM has remained instrumental in helping faculty and others get their technologies to market, growing from one-person office to an office of about two dozen today.
“The cooperation with OTM was incredibly important to the success of our discoveries,” he says.