The isolated living spaces of laboratory mice, especially those born with no exposure to bacteria, are a far cry from the way people actually live, whether home is in the suburbs of the American Midwest, the urban slums of Dhaka, Bangladesh, or the rural villages of Malawi. Nevertheless, studies of such mice — and the human gut bacteria they are given — have shed light on two of the major public health crises of our time — obesity and childhood malnutrition.
Spearheading efforts to understand the human gut microbiome is renowned researcher Jeffrey I. Gordon, MD, of Washington University School of Medicine in St. Louis. Gordon has been called the father of this field as well as, arguably, the most influential human microbiome scientist working today. Along with talented students and colleagues, Gordon has harnessed the power of specialized mouse models to study the microbial communities that colonize the human gut. Over the past 20 years, this work has revolutionized our understanding of human biology, implicating the gut’s microbial residents in orchestrating healthy growth and development when these communities work well, and in causing disease when they do not.
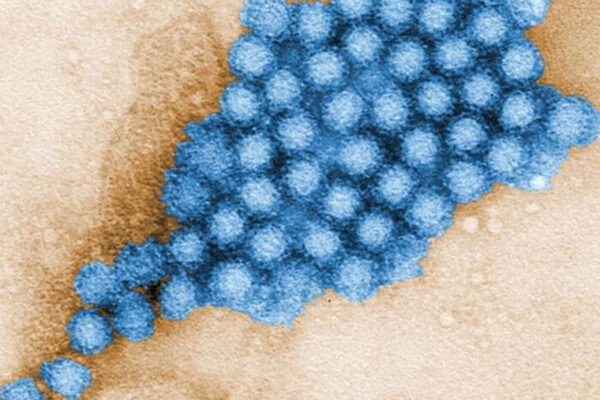
Gordon often speaks of the gut’s nonhuman residents — the microbiota — as a microbial organ. Like the body’s other organs, Gordon has shown, the microbiota performs specific and vital functions.
Gordon, the Dr. Robert J. Glaser Distinguished University Professor, directs the School of Medicine’s Center for Genome Sciences and Systems Biology. Over more than two decades, Gordon’s research has evolved from studying gut development from a human perspective to demonstrating that the human gut and its resident bacteria can’t be understood in isolation. Gordon often speaks of the gut’s nonhuman residents — the microbiota — as a microbial organ. Like the body’s other organs, Gordon has shown, the microbiota performs specific and vital functions. Without healthy development of the tens of trillions of microbes that make up this organ, the human gut does not work as it should. And this may have lifelong consequences.
The human gut also is a constant work in progress, with most cells of its inner lining renewing themselves every two weeks. The gut of a typical adult, including the large and small intestine, is more than 20 feet long, with different regions along its length performing different digestive tasks.
“In my final year of medical school, I was fascinated by a lecture series on the gut and the renewal of the cells lining the gut,” Gordon says. “Cells in different regions of the gut produce different products and perform different tasks. How do these cells know where they are along the length of the gut and what they should be doing? And how do they maintain this ‘positional’ identity over time?”
Seeking answers to these questions, Gordon and his students performed an experiment in which they used genetic methods to slow down the gut lining’s cellular renewal process in mice. Specifically, they made some of the cells, but not all, take longer to migrate from their birth place — the stem cell niche — to their final positions. During this migration, they normally differentiate to mature cells that perform key functions.
The researchers found that even though some cells took longer to get where they needed to go, they did not start performing their designated tasks earlier than they should. In other words, the cells were not relying on an internal clock, waiting on a particular time to elapse to begin their work. Instead, the cells lining the gut did not start doing their jobs until they were in the right place, no matter how long their journey took.
“These results spawned a debate in the lab — where to look for the source of this spatial information,” Gordon says. “As developmental biologists, it made sense to look at the gut’s underlying tissues for signals that guide the differentiation of these cells. But we could not ignore the fact that, beginning at birth, the gut is colonized by a vast microbial community. It was conceivable that these microbes could be sending key signals to the cells lining the gut.”
“As developmental biologists, it made sense to look at the gut’s underlying tissues for signals that guide the differentiation of these cells. But we could not ignore the fact that, beginning at birth, the gut is colonized by a vast microbial community. It was conceivable that these microbes could be sending key signals to the cells lining the gut.”
— Jeffrey I. Gordon, MD
Gordon credits the late David M. Kipnis, MD, who was head of the Department of Medicine when Gordon joined the Washington University faculty in 1981, with providing the support, trust and resources he needed to flourish as an independent research scientist. Gordon praised Kipnis for his willingness to take chances and provide long-term support for young faculty pursuing unconventional research.
“David was an inspirational mentor,” Gordon says. “He fostered the careers of several generations of physician-scientists because of his capacity to listen to them carefully at formative stages of their careers. He had the patience and wisdom to allow them to make the bold, unconventional investments needed to develop new technologies, create new model systems and acquire key observations, so they could succeed in the long term. He valued young people for their vision and commitment, and for their capacity to make future contributions, not just what they produced in the short term. He made arrangements in thoughtful and creative ways, so these young scientists would be placed in special environments that would be most supportive of their early development as independent researchers.”
In Gordon’s case, that special environment was in the Department of Biochemistry, where he established his lab while completing his clinical training in gastroenterology. He later became head of the Department of Pharmacology and Molecular Biology. And that is where his team began exploring the relationship between the gut and the bacteria that live there.
At the time, Gordon’s lab lacked the ability to breed mice under sterile conditions and strictly control the bacteria that end up in their pristine gut environments. But the Karolinska Institute in Sweden had such a “gnotobiotic” mouse facility. With the help of then-postdoctoral researcher Per Falk, who had done his doctoral studies there, Gordon teamed up with the Swedish researchers. Together, they conducted a series of experiments comparing gut development in germ-free mice to mice raised with normal exposure to microbes. The studies, performed by then-graduate student Lynn Bry, suggested that gut bacteria cause the cells of the gut to produce a type of sugar.
“Lynn found evidence that gut microbes are directing the host to serve them a meal of complex carbohydrates,” Gordon says. “The gut’s production of this ‘meal’ begins near the end of the small intestine and progresses along its length. This progression would begin in both the germ-free animals and in conventionally raised animals. But in sterile animals, this progression would stop around the time the mouse pups were weaned from their mothers.”
Bry then showed that if she added gut microbiota from conventionally raised mice to the just-weaned germ-free mice, their gut cells would begin producing these complex carbohydrates again.
But the microbiota of conventionally raised mice is extraordinarily complex. To tease out more details of the interaction between gut cells and bacterial cells, Gordon and his students needed a simpler system that would give them control over more variables. They chose to focus on a single type of bacteria, Bacteroides thetaiotaomicron, or B. theta, that was known to live in the human gut and to digest certain complex sugars that the human gut, lacking the proper enzymes, cannot break down.
“We felt that this dynamic of nutrient sharing was an extremely important foundation for establishing and maintaining mutually beneficial relationships between members of the microbiota and their host.”
— Jeffrey I. Gordon
The researchers found that B. theta alone could direct the gut to start this specific carbohydrate production program. But the program is dependent upon the organism’s ability to use that carbohydrate.
“We felt that this dynamic of nutrient sharing was an extremely important foundation for establishing and maintaining mutually beneficial relationships between members of the microbiota and their host,” Gordon says.
To gain insights into how B. theta was telling the gut to serve it a meal, Gordon and his students decided to sequence this bacterium’s genome. But they ran into a road block. At the time, in the late 1990s, major genome sequencing centers were not analyzing the DNA of friendly bacteria — they were focused on the human genome. So Gordon and his team took matters into their own hands and wrote a grant to purchase a DNA sequencer and set up a bacterial genomics pipeline in the lab.
“It took two years for us to sequence the entire genome of B. theta,” Gordon says. “But once we had the genome, we could start looking at the molecular foundations of the crosstalk between this bacterium and its host. We envisioned deliberately colonizing gnotobiotic mice with defined human gut communities composed of two, three, four or more sequenced bacterial members. These model communities could provide answers to basic questions about how microbes assemble in different regions of the gut, how they cooperate and compete, how different diets influence their behavior and how they, in turn, influence host biology.”
Gordon recalled thinking they could also colonize germ-free mice with intact microbial communities from people living in different parts of the world, with different lifestyles, ages and different states of health to determine the effects of these microbial communities on the recipient animals’ physiology, metabolism and immune function.
Armed with insights into the importance of B. theta and other gut symbionts, as well as in-house genomic sequencing tools and a new gnotobiotic mouse facility — built with support from then-dean of the School of Medicine, William Peck, MD — Gordon and his team began a systematic exploration of the ways bacteria interact with the gut.
In particular, they were interested in studying the role of the microbiota in human nutrition, starting with the opposite extremes of nutritional status — obesity and malnutrition.
Establishing cause and effect
Gordon and then-postdoctoral researcher Ruth Ley focused first on obesity and its associated metabolic dysfunctions. Their research showed that mice with a gene mutation that produced obesity, even with normal exposure to microbes, had a different mix of bacteria colonizing the gut than lean littermates with the same normal bacterial exposure but no mutation. This was true despite the fact that the mice were all born from the same mother and ate the same diet. Ley found that obese mice had fewer bacteria classified as Bacteroidetes and more classified as Firmicutes than lean mice.
In a paradigm-setting experiment that demonstrated how to distinguish whether this difference in bacteria was a cause or an effect of obesity, then-doctoral student Peter Turnbaugh showed that transplanting microbiota from the genetically obese mice into germ-free normal mice caused the recipient animals to become fatter than germ-free mice receiving microbiota from lean animals — even though all recipient mice were given the same diet and ate similar amounts of chow. At the same time, Gordon and Ley teamed up with Sam Klein, MD, the Danforth Professor of Medicine and an obesity researcher, to show that when obese humans consumed low-calorie diets, their gut microbiota changed as a function of their weight loss.
These lab results, described in two papers published in Nature in 2006, opened the door to thinking that microbial communities, not just single organisms, can cause disease. The discoveries were used by the National Institutes of Health as a justification for why a human microbiome project was needed and timely.
“We saw that the human microbiota could transmit features of obesity or leanness to these mice. We saw that microbiota from the obese co-twin transmitted features of obese humans — increased body fat and metabolic abnormalities — to these mice, while recipients of the lean co-twin’s microbiota were leaner and metabolically healthy.”
— Jeffrey I. Gordon, MD
Gordon and Turnbaugh also partnered with Andrew Health, DPhil, a Washington University professor who was conducting long-running studies of twins. Twins allow researchers to more easily separate the effects of genetics and environment. Their research showed that the gut microbiome of obese individuals lacks the diversity seen in the microbial communities of lean individuals. The lab’s genome sequencing capabilities also demonstrated differences in the genes present in these microbial communities, including genes related to metabolism and nutrient processing.
Going a step further, the researchers, led by then-graduate student Vanessa Ridaura, took stool samples from twin pairs where one was obese and the other lean. The microbiota of the lean and obese twins were transplanted into separate groups of gnotobiotic mice. All mice were fed the same amounts of food.
“We saw that the human microbiota could transmit features of obesity or leanness to these mice,” Gordon says. “We saw that microbiota from the obese co-twin transmitted features of obese humans — increased body fat and metabolic abnormalities — to these mice, while recipients of the lean co-twin’s microbiota were leaner and metabolically healthy.”
And in a tantalizing observation, researchers also showed that when these mice were housed together, which allowed them to share their bacterial strains, the microbes associated with leanness were able to establish themselves in the guts of the mice that had been given the microbiota associated with obesity. This invasion prevented the development of obesity and metabolic abnormalities in mice harboring the obese donor’s microbiota. Importantly — perhaps enough that it bears repeating — Gordon and his colleagues knew these mice were not consuming different amounts of food. The features of obesity were associated with differences in microbiota, not the number of calories consumed. Moreover, the invasion revealed that the lean donor’s microbiota would perform jobs that were completely missing from the microbiota of the obese donor. Filling these job vacancies appeared to prevent obesity from developing, Gordon noted.
The findings raise the prospects of future probiotic treatments for obesity. They also suggest that the nutritional value of foods cannot be determined independently of the microbes present in the gut and how they process nutrients.
The microbiota, Gordon and his colleagues have hypothesized, should be considered a component of the energy-balance equation. But even if gut microbes have their own say in calories in, calories out, more research is needed before this knowledge could be used to help reduce the burden of obesity on human health.
Nurturing a mature microbiota
At the opposite end of the metabolic spectrum, these observations also have profound implications for understanding malnutrition.
Similar to the studies that demonstrated a causal role for gut microbes in obesity, Gordon and his students have laid out evidence that the microbiota also bears some responsibility for childhood malnutrition, and the poor growth and development associated with it.
Their first goal was to document development of the microbiota in infants showing normal growth over the first several years of life, an undertaking led by doctoral student Sathish Subramanian and colleagues in Bangladesh. After establishing there is, indeed, a pattern of healthy microbiota development that is shared across individuals, Gordon and his colleagues compared these patterns to Bangladeshi children experiencing varying degrees of malnutrition.
Researchers found that malnourished children’s microbiota failed to follow the healthy pattern they identified in healthy children. Gordon’s work suggests the microbiota of malnourished children is immature, lagging in development behind that of their healthy peers. Supplementing these children’s meals with widely used therapeutic foods that increase calories and nutrient density reduces deaths from malnutrition, but it does not fix their persistent microbiota immaturity.
Perhaps more insidious than slowing growth is malnutrition’s effect on less visible aspects of health, including impaired brain development and dysfunctional immunity, which follow these children throughout their lives. Like with obesity, Gordon and his students, led by doctoral student Laura Blanton, replicated the microbiota of healthy and malnourished children in young gnotobiotic mice. Again, eating the same food — food that mimicked the ingredients and low nutrient content of the meals available to the children whose microbiota they harbored — these mice recapitulated features of normal growth or of impaired growth, depending on which microbiota they received. And the differences went beyond the size of the mice to include differences in metabolism in multiple organs and in bone development.
Their results provided preclinical proof that microbiota immaturity was causally related to malnutrition and that healthy growth is linked to healthy development of the gut microbiota. Their studies not only identified members of the microbiota that were positively correlated with growth, but also demonstrated how the microbiota’s effects extend beyond the gut. In addition, their findings underscore how the nutritional value of food is heavily influenced by the gut microbial community.
Searching for factors that might help establish a healthy microbiota and influence healthy growth, Gordon and his colleagues looked for clues in nature’s first food — breast milk.
Compared to the breast milk of mothers with healthy children, the researchers found that the breast milk of mothers with malnourished children had lower levels of sugars that carry sialic acid. To conduct mouse studies, Gordon and colleagues at the University of California, Davis used a similar compound found in cow’s milk, which they purified from the whey produced during cheese manufacturing.
Utilizing gnotobiotic mice with the gut bacteria of a malnourished child, the researchers, led by then-doctoral student Mark Charbonneau, showed that the animals receiving a low-nutrient diet supplemented with sialic acid from cow’s milk sugars showed improved growth, healthier metabolism and augmented bone growth compared to mice who received an unsupplemented diet with the same caloric density. These effects were dependent upon the microbiota: Germ-free mice who received sialic acid supplementation did not show improved growth.
As Gordon’s work has revealed the importance of the first few years of life and the exposures that shape the gut microbiota, he has turned his attention to identifying foods that can be given during the weaning period — when babies transition from mother’s milk to a typical diet — that will promote the development of a healthy gut microbial organ. With support from the Bill & Melinda Gates Foundation, Gordon is beginning to investigate such foods in children.
“We are designing these next-generation therapeutic foods from the inside out, guided by the gut microbiota.”
— Jeffrey I. Gordon
“We are designing these next-generation therapeutic foods from the inside out, guided by the gut microbiota,” Gordon says. “In addition to finding foods that support formation of gut microbial communities associated with healthy growth and development, it’s vitally important that these foods also are culturally acceptable as well as environmentally sustainable and affordable to produce.”
Continuing their collaboration with the International Centre for Diarrheal Disease Research in Bangladesh, Gordon and his team will set up the first study site in Mirpur, located in the Bangladeshi capital city of Dhaka. The goal is to investigate whether these foods can durably repair the immaturity of the gut microbiota seen in malnourished children, especially those who have remained stunted and underweight even after having been treated with current therapeutic foods.
“We hope these studies will lead to food-based interventions for undernutrition that produce better clinical outcomes,” Gordon says. “Looking beyond malnutrition, the lessons learned may provide more informed and generalizable recommendations for feeding practices during the time infants are being weaned.”
The researchers are proceeding with caution, first with food-based therapies. In the future, according to Gordon, treatment of severely immature microbiota may also have to include administration of next-generation probiotics, consisting of defined collections of beneficial bacterial strains cultured from the human gut microbiota.
“There is a window in human postnatal development of the microbial organ that we may be able to modify in ways that promote long-term health,” Gordon says. “We need to consider not only the biological implications, but also the societal issues raised by these efforts.”
Gordon often speaks of the complexities of this work that go far beyond laboratory mice, including the need to form partnerships with local communities and with specialists in other important areas, including agriculture, food science, public health and business. Such expertise and partnerships are required whether seeking ways to empower mothers who may be struggling to breastfeed or ways to create local food-based industries. These industries should simultaneously support the economic health of a community and the healthy growth of its children, all while respecting cultural and culinary traditions.
Gordon’s idea of partnerships also extends beyond the human and into the microbial world.
“Being able to see ourselves as a splendid collection of interacting human and microbial parts teaches us that we do not travel through life alone, unaccompanied,” he says. “There is a microbial dimension to our development that offers an expanded view of the ‘self.’ Studying this expanded view of ourselves offers the possibility of entirely new approaches to human well-being.”
Julia Evangelou Strait is a senior medical science writer in Medical Public Affairs.